Does COVID vaccination reduce COVID mortality?
The data is available so why don't public health authorities use it?
I wonder, is there really no-one in public health who can do simple stats? I’m no expert but I did pay attention in Econometrics 1.01. I’m going to try and put what I learnt to good use even though I’m a little rusty.
Two things I do remember well:
High R-squared indicates the variable explains a lot of the variance.
Low P-value means the variable is statistically significant.
Despite being funded by Bill Gates, those good people over at Our World in Data provide some really useful data in addition to all the COVID metrics like deaths and vaccination data. But no-one ever seems to make use of it, not the public health authorities, the so-called “experts” used by governments or the mainstream media.
They do, however, keep trumpeting the mantra “vaccines are SAFE and EFFECTIVE”. I have covered the “safe” aspect before and will do so again in other posts but for this one, I’m going to focus on the “effective” part.
With up to 95% claimed effectivenes, it should not be difficult to observe a material impact on reported COVID mortality, should it?
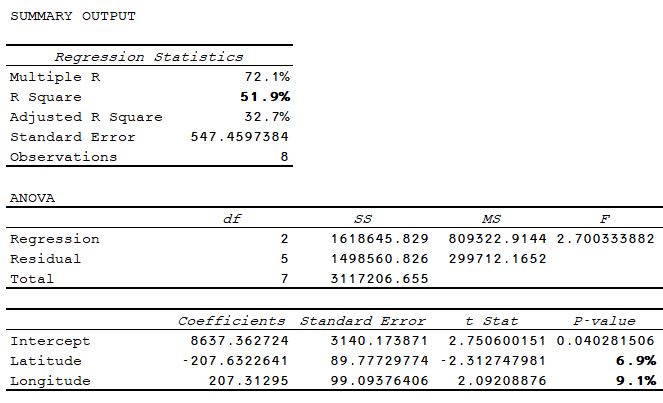
I have chosen a cohort of mid/east European countries to try and minimise any confounders of physical geography. On 30-Nov-21, all had substantial levels of COVID deaths.
Despite geographical proximity, looking at the regression between COVID deaths per million and geographical coordinates, we can explain half the difference in deaths already. And assuming a statisitcal significant cutoff of 5% in the P-value, we aren’t far off either.
Still, let’s press on and do the same exercise with vaccination rates.
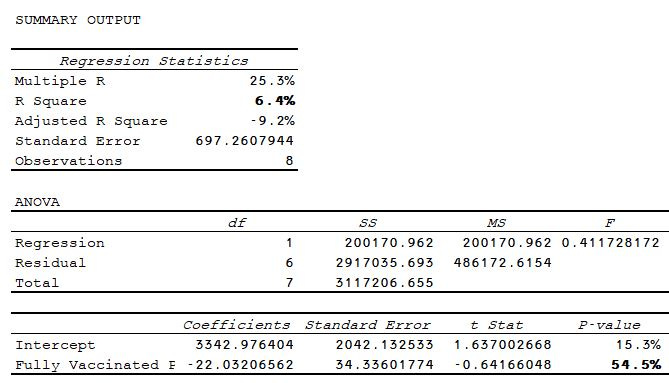
The vaccination rate ranges from just over 40% to just under 70% of the population. This ought to be enough to show some impact on mortality. Evidently, it does not.
With a P-value of over 50%, the stats show us without doubt that the rate of fully vaccinated population has no statistical signifcance on the level of COVID mortality across these countries on 30-Nov.
So, if COVID vaccines don’t affect COVID mortality and physical geography only explains a part of the story, are there any other variables we can examine?
It’s always best to start with your intuition, so I chose:
Population Density;
Population Aged 70+;
GDP per Capita;
Extreme Poverty;
Cardiovascular Death Rate;
Diabetes Prevalence;
Hospital Beds; and
Life Expectancy
Only four data that showed any evident correlation in single linear regression.
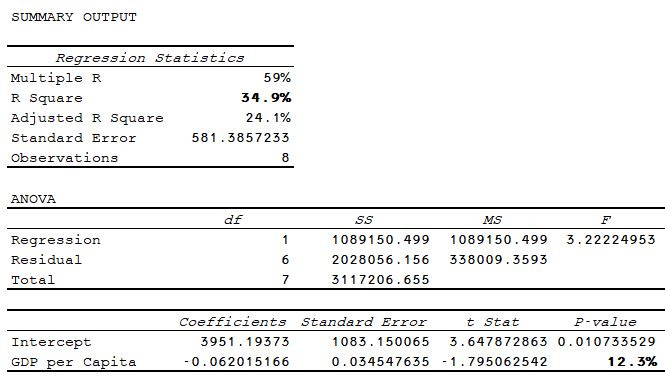
As you would expect, GDP showed a negative relationship, i.e. the higher the GDP per Capita, the lower the COVID death rate.
With a P-value of 12%, this variable is not statistically significant on its own but again quite demonstrably more so than vaccination rates.
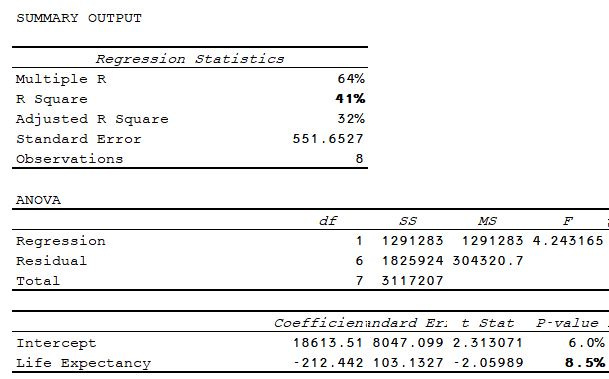
Not surprisingly, life expectancy shows the same negative relationship. COVID does substantially affect very old, frail people more than any other goup after all. Something we have known since Feb 2020!!
With a P-value of 8.5%, it is not far off being significant either, getting clsoer to the ubiquitous 5% cutoff.
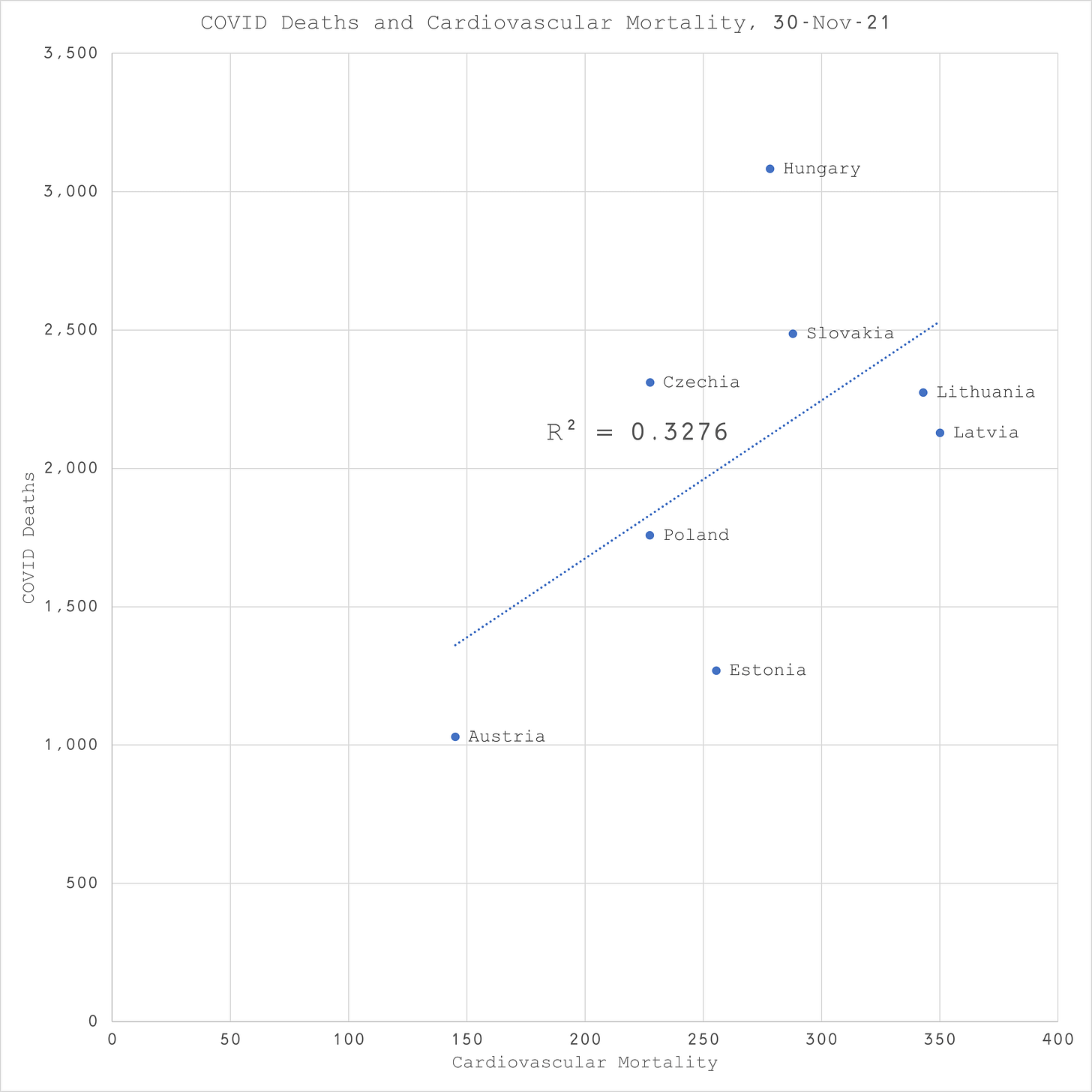
Background cardiovascular rates appears to have a similar explanatory power to GDP. This time, as expected, the relationship is positive, i.e. the higher the background rate of cardiovascular mortality, the higher the rate of COVID mortality.
The same is true of diabetes prevalence to a lower extent.
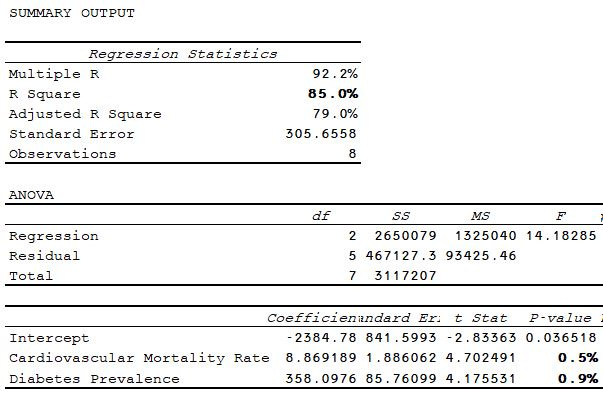
But what happens if you combine these two important markers of background health in a multiple linear regression (ooops, might have slipped into Econometrics 1.02 there)?
Well, would you look at that? Just these two variables on their own explain 85% of the variation in COVID mortality and both have P-values below 1%. This is significant! Both in terms of statistics but more importantly in terms of public health policy, isn’t it?
If COVID mortality is so strongly correlated with background rates of cardiovascular mortality and diabetes prevelence, doesn’t that indictae where public health authorities ought to be looking for the “cure”? Because, the vaccine certainly isn’t it.
Imagine how many lives really could have been saved if all the resources wasted on COVID measures and vaccines had instead been channelled into reducing the factors that influence cardiovascular disease and diabetes instead? You know, like healthy eating, exercise and low stress. Many of the opposite things achieved by lockdowns and community mask wearing.
Maybe my original premise was wrong and this is not about public health after all?